Navigating India's Mental Health Terrain: From Large Metros to Smaller Towns
/Mental Health Definition
The World Health Organization (WHO) defines mental health as a state of overall well-being where individuals recognize their abilities, handle everyday stresses effectively, engage in meaningful activities, and positively impact their communities. Good mental health underscores the need for adequate psychiatric resources to ensure that individuals have the necessary support to maintain such a state of well-being.
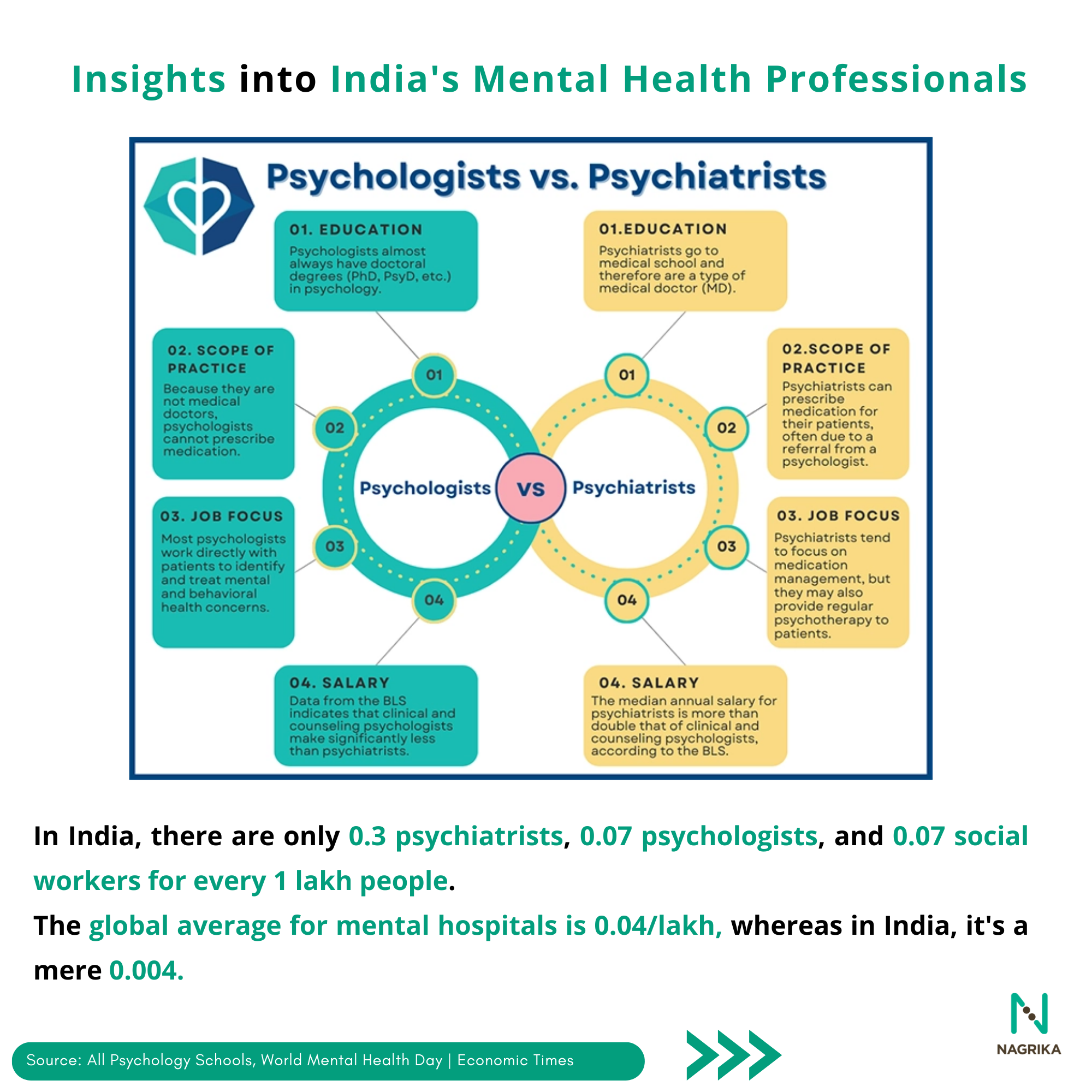
The WHO recommends having 3 psychiatrists and 1.5 psychologists for every 1 lakh people. However, in India, there is less than 1 psychiatrist for every 1 lakh people. According to the Ministry of Health and Family Welfare, India currently has 898 psychologists, which falls short of the required 20,250. Less than 10% of the 50 million people with depression in India receive adequate care, and almost no one has access to evidence-based psychological treatment. The lack of awareness and the shortage of mental health professionals has resulted in numerous patients being unable to access medical assistance. There is a significant gap in mental health services in non-metropolitan and rural areas, resulting in a 95% treatment gap for common mental disorders.
A survey conducted by the LiveLoveLaugh Foundation uncovered distressingly insensitive and uninformed perspectives on mental health in India. Majority of people believe that people with mental illness lack self-discipline. This creates a harmful cycle of shame, distress, and social isolation for those affected. Dr. Swapnil Lale, Additional Director of Health Service in Maharashtra, highlights that due to such stigma, people in India still fear visiting a psychiatrist.
Leveraging medical technology will be essential in addressing the shortage of mental health professionals, with strategies such as telemedicine, virtual care, and smartphone applications being pivotal. Additionally, there is a growing trend of training grassroots medical workers and community-led solutions to address mental health challenges.
Does living in cities affect our mental health?
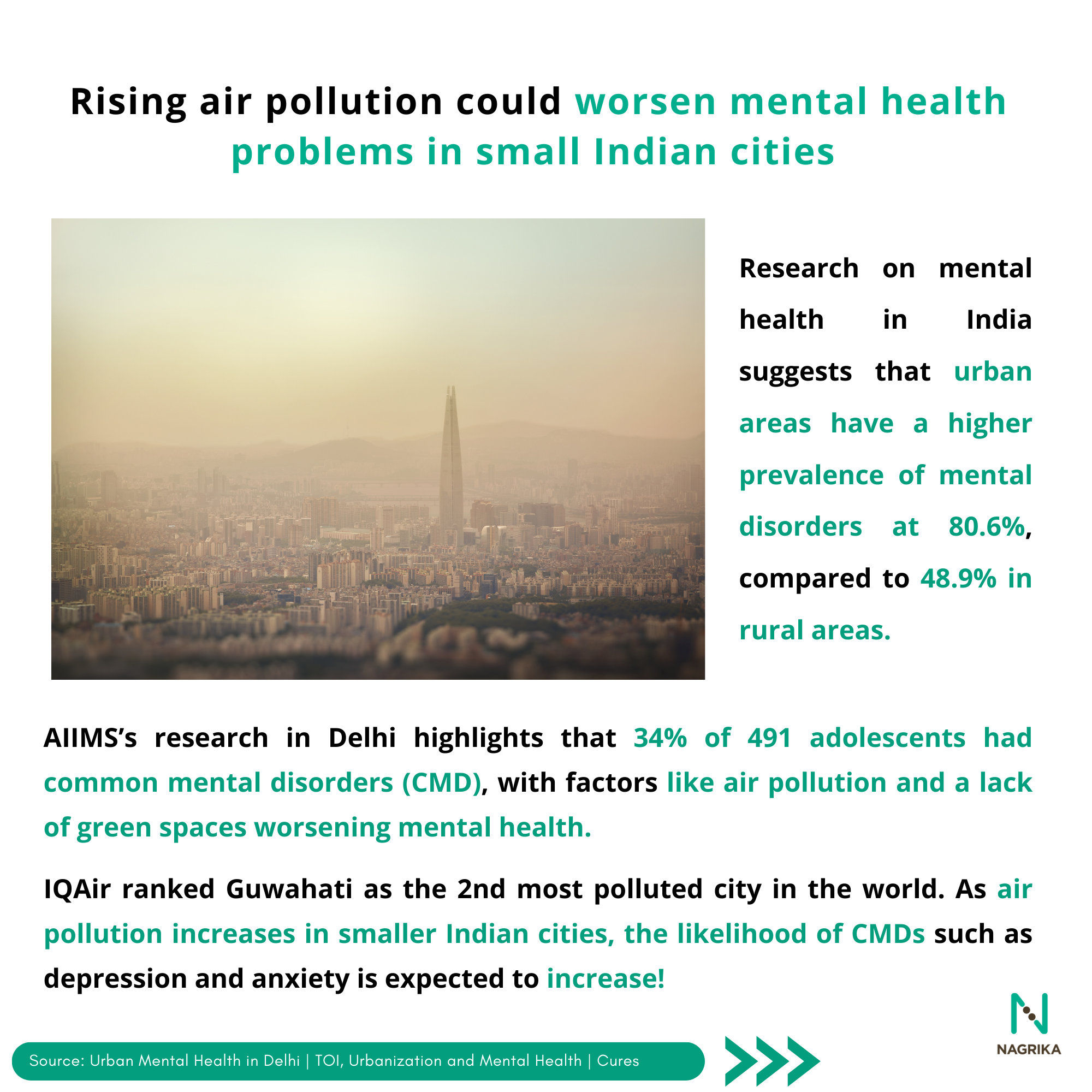
As per the Centre for Urban Design and Mental Health, cities tend to have elevated rates of various mental health issues compared to rural areas. This includes nearly a 40% increased likelihood of depression, over 20% higher rates of anxiety, and double the risk of schizophrenia, along with feelings of loneliness, isolation, and stress. Indian epidemiological research on mental health disorders reveals that the prevalence of mental illnesses ranges from 48.9% in rural areas to 80.6% in urban areas. Rural India also struggles with undiagnosed mental illnesses due to stigma, lack of awareness, and scarce access to mental health professionals.
In urban areas, inadequate green areas, pollution, urban heat islands, and a lack of pedestrian and cycle-friendly infrastructure further exacerbate mental health problems. AIIMS conducted a study in Delhi, reporting that 34% of 491 adolescents had common mental disorders (CMD), with factors like pollution and lack of green spaces worsening the situation. IQAIR reports 15 out of the world's top 20 polluted cities are small and mid-sized Indian cities. As pollution rises in smaller Indian cities, the likelihood of CMD such as depression and anxiety is expected to increase.
Smaller cities like Kota and Thrissur have also seen clusters of suicides, likely influenced by the presence of coaching institutes focused on competitive exams. According to NCRB 2021, Maharashtra reported the highest suicide cases, followed by Tamil Nadu, and Madhya Pradesh. Cities like Prayagraj, Varanasi, Mainpuri, and Meerut in Uttar Pradesh are witnessing a rise in severe mental disorders and individuals at risk of suicide.
Depression, anxiety, and suicide rates tend to inversely correlate with income and employment levels. Individuals with the lowest incomes within a community experience depression, anxiety, and other prevalent mental health issues 1.5 to 3 times more frequently than those with the highest incomes. This uneven impact highlights the urgent need to examine the working conditions and mental health of those in lower-income brackets, as these factors are closely linked to mental health outcomes. Paigam, in partnership with the Indian Federation of App-based Transport, conducted a survey across 8 cities in India, revealing that a significant portion of workers labour for over 10 hours daily and earn less than Rs. 15,000 per month which causes dissatisfaction.
Insights into India's Mental Health Landscape: Challenges, Gaps, and Government Initiatives
The 2016 National Mental Health Survey (NHMS) reports that about 10% of India's population require direct interventions for mental health issues in India. According to the National Rural Health Association, accessibility to mental health services, availability of mental health professionals, affordability to better private mental healthcare, and acceptability to receiving mental healthcare are major challenges in smaller towns and rural areas of India.
The NMHS also revealed that the general occurrence of Common Mental Disorders (CMDs) in India stood at 5.1%, with a treatment gap of 80.4%. Mental disorders except epilepsy, recorded a treatment gap of more than 60%, with the highest being for alcohol use disorders at a shocking 86%. The National Crime Records Bureau (NCRB), reports that the percentage of suicides linked to alcohol and substance use rose from 5.2% in 2017 to 6.8% in 2022.
To enhance mental healthcare accessibility, the Government launched the National Mental Health Programme (NMHP) along with the District Mental Health Programme (DMHP), approved for 704 districts through the National Health Mission. The state governments have also launched various schemes to strengthen the access and affordability to Mental Healthcare. The Government of Gujarat has launched a toolkit called ‘WHOQR’, for training mental health professionals for awareness generation, early detection and reduction in treatment gaps. Pilot programs like Suicide Prevention & Implementation Research Initiative (SPIRIT), and Atmiyata, for mental healthcare in Mehsana to enhance the accessibility to mental health services for vulnerable populations. The launch of the National Suicide Prevention Strategy (NSPS) in 2022 marks a significant initiative geared towards systematically tackling the multifaceted causes of suicide and striving for a 10% decrease in the country's suicide rates by 2030.
Increasing Access to Mental Healthcare in Smaller Towns through Tele-Mental Health Services
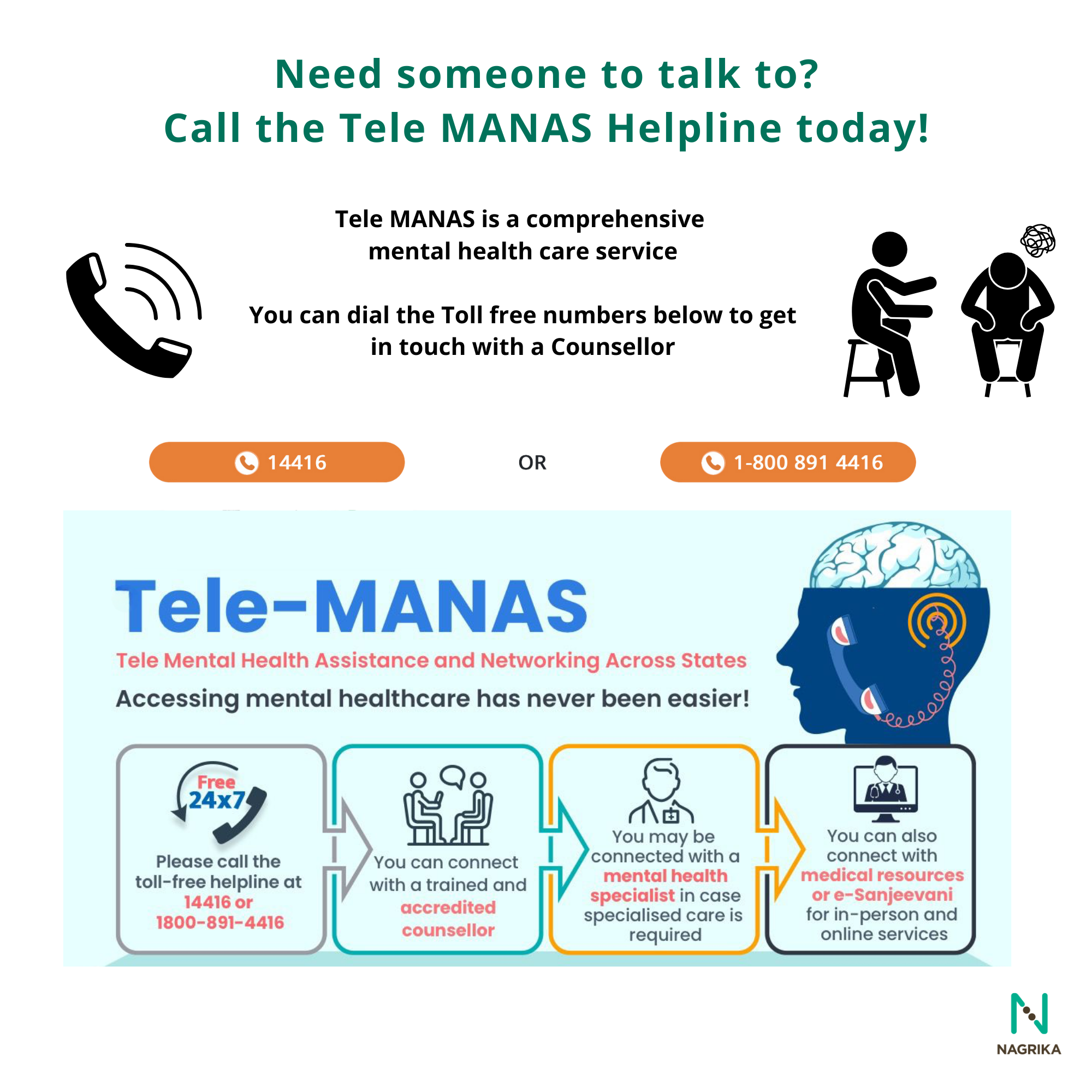
Besides the above, the government has introduced a "National Tele Mental Health Programme" in the 2022-23 budget to enhance accessibility to high-quality mental health counselling and care services. Tele MANAS, the National mental health helpline, since its launch in 2022 has received more than 18,000 individuals from Maharashtra out of which 30 percent of these callers originated from small and intermediate cities such as Kolhapur, Pune, Sangli, Aurangabad, and Mumbai. In 2023, AIIMS-Bhopal provided mental health treatment to 38,000 patients through 'Tele Manas'.
‘‘Rocket Health,’ a digital intervention initiated by Abhineet Kumar and Dr. Ritika Sinha for COVID patients, now also offers therapy and psychiatry sessions, psychologist-led support groups, peer groups, and mental health assessments. About 50% of app users are from Tier-2 and Tier-3 cities. Likewise, Wysa, an AI-driven mental health support provider, announced the launch of its conversational AI in Hindi, which aims to significantly improve access to quality services in Tier 2 and 3 cities across India.
Bridging Mental Health Gaps: Community Empowerment and Advocacy Initiatives in India
Meanwhile, ASHA workers are playing a significant role in bridging mental health gaps in smaller towns and rural areas. In Gurgaon, about 1000 ASHA workers have screened over 4000 people for depression out of which 1300 patients were screened for counselling at government hospitals. The Madhya Pradesh government, in collaboration with NGO Sangath, has empowered ASHA workers to serve as the first responders for individuals facing mental distress in Raisen, Vidisha, and Narmadapuram.
The National Educational Policy 2020 underscores the significance of prioritising the mental health and emotional wellness of students. While implementation of the NEP varies across regions, it is gradually tackling mental health concerns at a local level, extending its reach to Tier II and Tier III cities. Mind and Matter, an organisation based in Mysuru advocates to prioritise mental health among children in Madikeri. Since November 2023, they have been conducting awareness campaigns in schools across Mysuru and Kodagu.
The LiveLoveLaugh Foundation and the Association for People with Disability has successfully established a self-sustainable, community-driven mental health intervention in Devanagare, Karnataka. Launched in 2016, this Community Mental Health Programme adopts a strategic combination of activities, including street plays, wall paintings, and continuous training for frontline mental healthcare workers to raise awareness and improve access. The Schizophrenia Research Foundation (SCARF) initiated the 'Manam Inidhu' program, modelled after ASHAs, to extend community mental healthcare. This involved training women from self-help groups in fundamental mental health principles and counselling.
May 2024 is Mental Health Awareness Month, shining a spotlight on the theme "Movement: Moving more for mental health." This month serves as an opportunity for everyone to deepen their understanding of mental health, dispel myths, and embrace truths! Let us know in the comments section below!